Climate change is among the leading global health threats of the 21st century. Its impact on health is complex and varied, and it will exacerbate the burden of every major health-outcome category: infectious diseases; chronic diseases; mental health; injuries; and deaths.
Climate change also will affect health and life sciences stakeholders via more frequent and severe disruptions, as well as acute climate-related hazards, also accumulating strains on demand, capacity and finances due to chronic hazards and their lasting or lagging effects.
The health and life sciences sector is part of the problem — if the sector were a country, it would be the fifth-largest emitter of greenhouse gases on earth, mainly due to production, transport and disposal of products and services across the health supply chain. The sector is also a crucial part of the solution, with both an obligation and an opportunity to mediate the health impacts of climate change and minimize harms and inequities for patients, staff and societies.
Climate is a threat multiplier for health
Mortality risk is rising. Annual heat-related deaths could increase ninefold in the U.S., from about 12,000 now to more than 100,000 by 2100 in a high-emissions scenario. Intensifying storms also could increase the risk of deadly health care disruption, similar to that faced by Puerto Rico in 2017 — when one-third of casualties in the three months after Hurricane Maria may have occurred because medical care was disrupted or delayed.
Injuries could increase. Some 26 million people across the Philippines, Indonesia and Malaysia may be exposed to injuries during storm surges by 2045 in a high-emission scenario, as coral bleaching weakens a natural defense against coastal erosion, storms and floods in low-lying coastal areas.
Infectious diseases may expand or (re)-emerge. Dengue could spread to the Southeastern U.S. by 2050 as mosquito transmission zones expand from the tropics. Arctic heatwaves are thawing permafrost and could revive long-dormant pathogens, such as bacteria and viruses that cause anthrax, smallpox or the 1918 influenza pandemic.
Chronic disease prevalence, related vulnerabilities and costs could increase. Longer and more severe fire seasons expose more people to smoke: The 2019 Black Summer bushfires affected 80 percent of Australia’s population; survivors may face increased risks of cancer and respiratory and heart disease. Health costs accounted for more than half the total cost of the fires.
Mental illness may surge. Among Pacific Islanders at risk of forced displacement as sea levels rise, and among Central American migrants fleeing droughts, hunger and poverty, more than half the population exhibits signs of mental ill health — more than double the global period prevalence, serving as a potential glimpse into the future for other places in the world.
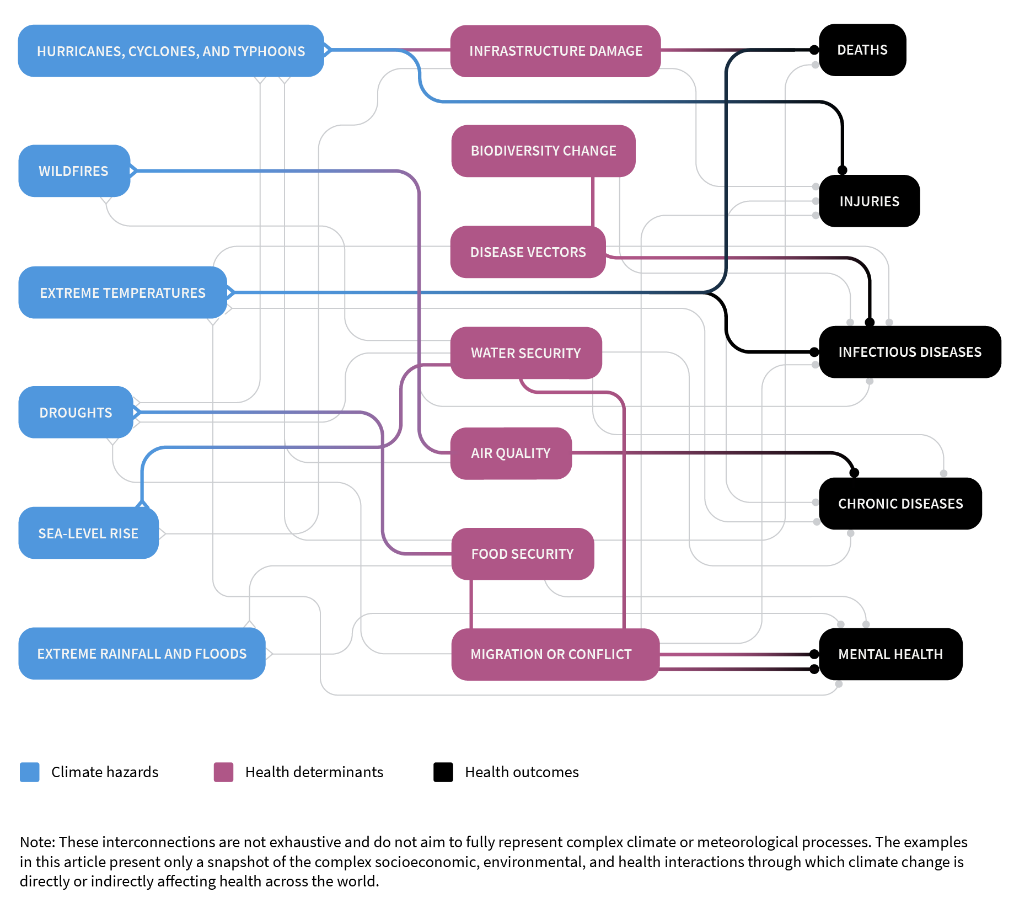
Climate-sensitive events and trends harm health directly, but also indirectly by altering interdependent pathways that act as environmental, social and economic determinants of health. For example, more frequent and intense storms can inflict more injuries (a direct result); but they also can increase mortality by disrupting urgent and essential medical care (an indirect effect).
Exhibit: Climate change affects health directly and indirectly through complex pathways
Source: Marsh & McLennan
Climate impacts on health range from mild to severe and from acute to chronic. Wildfires and floods cause initial spikes in physical and mental health needs, followed by lasting ill health that, over time, accounts for the bulk of consequent health care costs and productivity loss. Risks and outcomes once perceived as far off in time or space are unfolding and will intensify in both developed and developing countries.
Wildfires and floods cause initial spikes in physical and mental health needs, followed by lasting ill health.
Health and economic disparities also are exploited and widened by climate change, because the people and places worst hit are least capable of coping. For example, the elderly, the poor and people with pre-existing conditions face greater mortality risk during heatwaves.
Rising temperatures and sea levels threaten lives and livelihoods in tropical islands and regions, undermining their capacity to respond to catastrophes for which they are least responsible.
Building resilience
To date, the health and life sciences sector has been slow to respond — it historically has perceived impacts to be distant or uncertain and has deferred systemic changes. To reduce health risks and costs for the communities they serve, health care providers, payers, life sciences companies, employers and policymakers must ensure continuity of care during crises and prepare for changing needs for health care.
Hospitals and other providers must prepare for spikes in urgent care needs, volatile elective care, capacity disruptions and cost pressures. They should invest in infrastructure resistant to extreme weather, create surge capacity for essential resources (including staff) and plan for effective coordination with other stakeholders during crises. Providers also can devise adaptive service and staffing models such as telehealth and enhance community resilience by supporting public health measures to improve well-being and equity.
Health insurers and government payers face unpredictable and unmanageable claims and costs, a widening health protection gap and asset volatility for investments exposed to risks. Payers need to develop products or models that ensure universal access to physical and mental health care as well as determinants of health (such as food, housing, education and financial security).
Life sciences companies have opportunities to counter new health threats and to anticipate growing risks — such as physical disruptions, pricing and patent challenges as health care costs soar, and biodiversity loss that shrinks sources of existing and potential drugs. Pharmaceutical and medical device companies can reconfigure operations and supply chains for greater resilience, align research with changing disease burden and invest in rapid-response capabilities and partnerships (such as to repurpose drugs or discover vaccines). They also must ensure universal access and affordability for essential medicines and supplies.
Employers will experience spikes in care needs and costs that may coincide with health care disruptions, productivity loss and economic strain. Employers can reduce health and safety risks for workers by modifying work sites, schedules, practices, equipment and exposures. As payers, employers should design leave and health benefits to ensure all workers receive necessary care — especially low-paid and migrant workers, who are more vulnerable to climate hazards. They also can bolster workers’ resilience by improving work-related determinants of health, such as financial well-being.
Policymakers can minimize health impacts of climate change by strengthening health systems and building national and community resilience — for example, by integrating health impacts into disaster planning and risk reduction. They can implement policies with co-benefits for health and promote universal access to basic services and determinants of health. Policymakers also can spur investment and innovation now to monitor, avert and respond to future crises — for example, disease surveillance to prevent pandemics or vaccine platforms for rapid response.
Reducing emissions
All stakeholders have room to reduce their carbon footprint. For example, providers and life sciences can switch to renewable energy sources and low-carbon technologies; payers and employers can prefer sustainable providers of products and services as well as channel investments into green assets; the sector can use its trusted voice to educate communities on climate risks and solutions; and policymakers can drive climate mitigation and adaptation efforts for immediate and long-term health benefits.
The health sector must strike a balance between efficiency and resilience by cutting emissions and costs without sacrificing quality or continuity of care. Some changes will increase efficiency and resilience, while other options present trade-offs. One lesson from COVID-19 has been the cost of inaction and the value of preparedness, prompt response, resilience and coordination.
Given the threat of climate change to health and the lag between emissions and consequences, urgent action is vital. The right responses today will go a long way toward reducing risks and the need to make even more drastic and expensive changes tomorrow.