The glue inspired by a worm could save your life someday
Biomimicry in the making of a surgical glue: scientists seek the sticky, wet, and adhesive properties of worm secretions in creating a medical glue for surgery.

Materials scientists and engineers are discovering the secrets of organic substances and their properties and applying them to difficult challenges such as minimally invasive surgery. One such team appears to be on the cusp of a successful new medical adhesive inspired by the sticky secretions of a marine worm. But the journey from scientific discovery to commercial success has been paved with the work of many and has ranged widely from the recipe used by the worm. And it is far from over.
The inspiration: the Sandcastle worm
The Sandcastle worm (Phragmatopoma californica) is a Pacific Ocean polychaete worm that exists in the dynamic environment of the intertidal zone. As part of its strategy for survival against the mechanical forces of waves and the prying of predators, the worm uses a glue to affix bits of shell and sand particles together to make a tube home. Colonies of these tubes can be several meters across. During the exposed low tide the worm remains beneath its operculum seal and, when the tide is in, the worm extends its tentacles to catch food within the water. It is not alone in using an underwater glue; mussels, oysters and barnacles all use this strategy in the marine environment.
The makeup of this glue has been an object of research for some time and in 2005 a team from J. Herbert Waite’s lab at the University of California, Santa Barbara, was able to sequence the protein structure of this bio-adhesive and describe how it sets. Not surprisingly, the proteins are similar to that found in mussel byssus and belong to a small group called the polyphenolic proteins. The glue as made and dispensed is very much like a two-part epoxy, with proteins and associated adhesion-forming side groups formed separately and then mixed as they are secreted from a gland. The glue sets underwater in 30 seconds and cures in about six hours. Researchers think that the setting is triggered by the meeting of the acidic protein mix and the base seawater.
In 2009, Russell J. Stewart’s lab at the University of Utah was able to make a synthetic version of the glue. This group was able to achieve similar results without slavishly imitating the chemical structure of the natural version. The combination of side chains for cross-linking and the forming of a complex coacervate, a hydrophobic array, was important in developing this viscous, immiscible liquid.
The application development
Jeffrey M. Karp’s group reported their development of a new type of surgical glue in the January 2014 issue of Science Translational Medicine, “A Blood-resistant Surgical Glue for the Repair of Vessels and Heart Defects.” Its stated goal was developing a nontoxic, strongly binding adhesive that could work in the wet and dynamic environment of surgery. This was to improve minimally invasive reconstructive cardiovascular surgery. Key design criteria were that its substance would be a “biomimetic, stable, water-insoluble precursor that could resist washout in vivo, be cured in situ via light activation, and achieve a water-tight but flexible bond.”
Karp is a bioengineer at Brigham and Women’s Hospital in Boston, an associate professor in Medicine at Harvard Medical School and on the faculties at the Harvard Stem Cell Institute and MIT. He is also the co-founder of Gecko Biomedical.
He and his team are keen to improve the techniques in surgery, particularly by using adhesives for tissue repair rather than traditional staples. This is an extremely challenging environment in which to glue something: crowded wet spaces with highly flexible tissues in constant movement and the practitioners under critical time constraints.
Current clinical methods include the use of medical-grade cyanoacrylate (“super glue”) or fibrin sealant and both have serious drawbacks, being either toxic or weakly adhesive and prone to be washed out by blood flow before being affixed. Other adhesives under development depend on specific chemical interactions that make their applications limited, and their catalyzing sequences make prepositioning difficult.
While the group mentioned initial inspiration from several animal-inspired formulas including the synthetic glue inspired by the sandcastle worm, it chose for its base a synthetic adhesive it had developed as a biocompatible elastomer in 2007, poly(glycerol sebacate acrylate), PGSA. It contains components already in the human body: glycerol is a foundational component for lipids and sebacic acid is a metabolic intermediate for fatty acids. Both are approved by the U.S. Food and Drug Administration. PGSA can be photo-cured in five to 30 seconds, making it a good candidate for medical procedures.
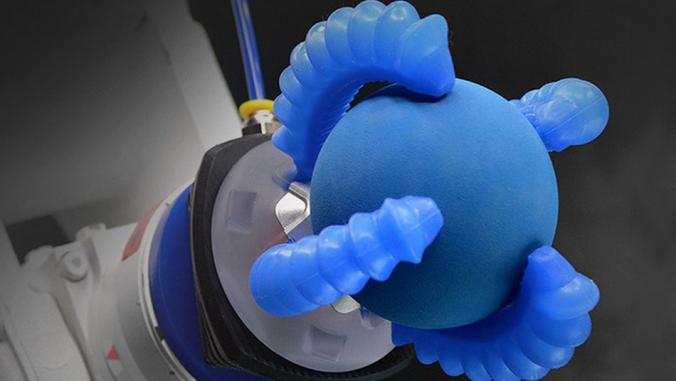
The result of the group's experimentation was a hydrophobic light-activated adhesive (HLAA) made up of the PGSA precursor and a photo initiator. It tested this in vitro and in vivo using, among other things, pig tissue and rat hearts. It reported excellent biocompatibility, good adhesion to soft tissue and, importantly, no washout or degrading of the adhesive properties due to blood flow. The advantages over current methods and materials were many, because no procedures allow positioning of hydrophobic prepolymers and such quick curing, which avoids potential damage from light-sourced heat. Moreover, the researchers claim to be able to tune the mechanical properties of the substance by adjusting its formula and controlling cure time and light intensities. Recently, the researchers have been able to scale manufacture of the adhesive by 100x, and intend to test it in live pigs in 2015.
The market
The performance success of the HLAA is buoying the prospects of Karp’s new company, Gecko Biomedical, a Paris-based biotechnology startup. Gecko Biomedical is privately owned and has been funded by a group of investors that include Omnes Capital, CM-CIC Capital Innovation and CapDecisif Management. It also has received funding from the French government. The money will be used to develop further Gecko's line of “Bioinspired Surgical Solutions.”
The company is a confluence of the scientific talent at MIT, namely Robert Langer and Karp; the iBionext Network, founded by Bernard Gilly and centered in Paris around the Institut de la Vision; and the capital investors.
The market focus for the company is minimally invasive procedures, where an instantly curable glue that can stand up to the demands of the in vivo environment has great advantages. As described in the above scientific paper, the HLAA also might become a new standard option for all sorts of tissue repair.
Much remains to be done before this glue becomes a regular feature of operating rooms. Its development is in the pre-clinical trial position, meaning that it has not been tested on humans yet, but the company has scaled the material for production, stabilized the formulation and intends to begin human trials in 2015 or early 2016. New formulations, fine-tuning of characteristics such as viscosity and adhesive strength and an exploration of how to better incorporate bioactive therapeutics into the mix are all ongoing. Beyond that, toxicity and safety studies will have to be done to pave the way for the clinical phases. One possible early path to human testing envisioned by the inventors has been as a hemostatic agent for suture line bleeding or small lacerations, because the glue seals so well. This more limited performance and safety testing might come before the more complex and longer-term studies needed for internal tissue repair such as patches to the heart.
The initial curiosity of naturalists, the field study and analysis of scientists, the development of a synthetic alternate by chemists and development of a useful application by biomedical engineers all have contributed to bringing this innovation to within reach of the market. While it is impossible to know how successful the next phase of development will be, it is an encouraging story of how science can tap nature for the human good.